Let’s start with the problem. Millions of FBDE (Full Benefit Dual-Eligible) individuals experience both physical and behavioral health disabilities – creating difficult barriers to accessing the care they need.

Low member engagement culprits: 3 barriers to navigating care
The ‘dual’ in Dual Special Needs
When members qualify for care management, they are often assigned two different care managers for their Medicaid and Medicare services. Many times Medicaid covers their behavioral health services while Medicare covers medical services. On top of the split between Medicaid and Medicare systems, D-SNP members may also face being covered under two unassociated plans, for example, Cigna versus UnitedHealthcare.
Needless to say, navigating not one, but two health plans for various care needs makes access to services a more complicated and aggravating process for the member. While members struggle, payers are faced with compensating through cost-shifting strategies to rebalance the public and private sectors as a result of duplicated services and additional revenue loss.
Greater social risk factors
In addition to the challenges of Medicaid and Medicare service coordination, health disparities and inequity are exceptionally prevalent among dual eligible individuals, creating a higher disadvantage for social risk. External components such as socioeconomic, racial, gender, age, and environmental influences diminish opportunity for D-SNP members to successfully care for their health and engage in their plan. These individuals are often challenged by SDoH (Social Determinants of Health) needs such as:
Between an inability to read prescription drug instructions and the anxiety of securing weekly meals, payers recognize that social barriers to care undoubtedly contribute to poorer health outcomes and, in turn, avoidable ED service utilization.
Plans have started placing greater focus on SDoH needs to ensure members are adequately served from a whole-person care perspective. The challenge is capturing needs in the moments outside of the traditional care setting, which contribute to about 80 to 90 percent of member health outcomes.4
Higher illness susceptibility, soaring COVID hospital utilization
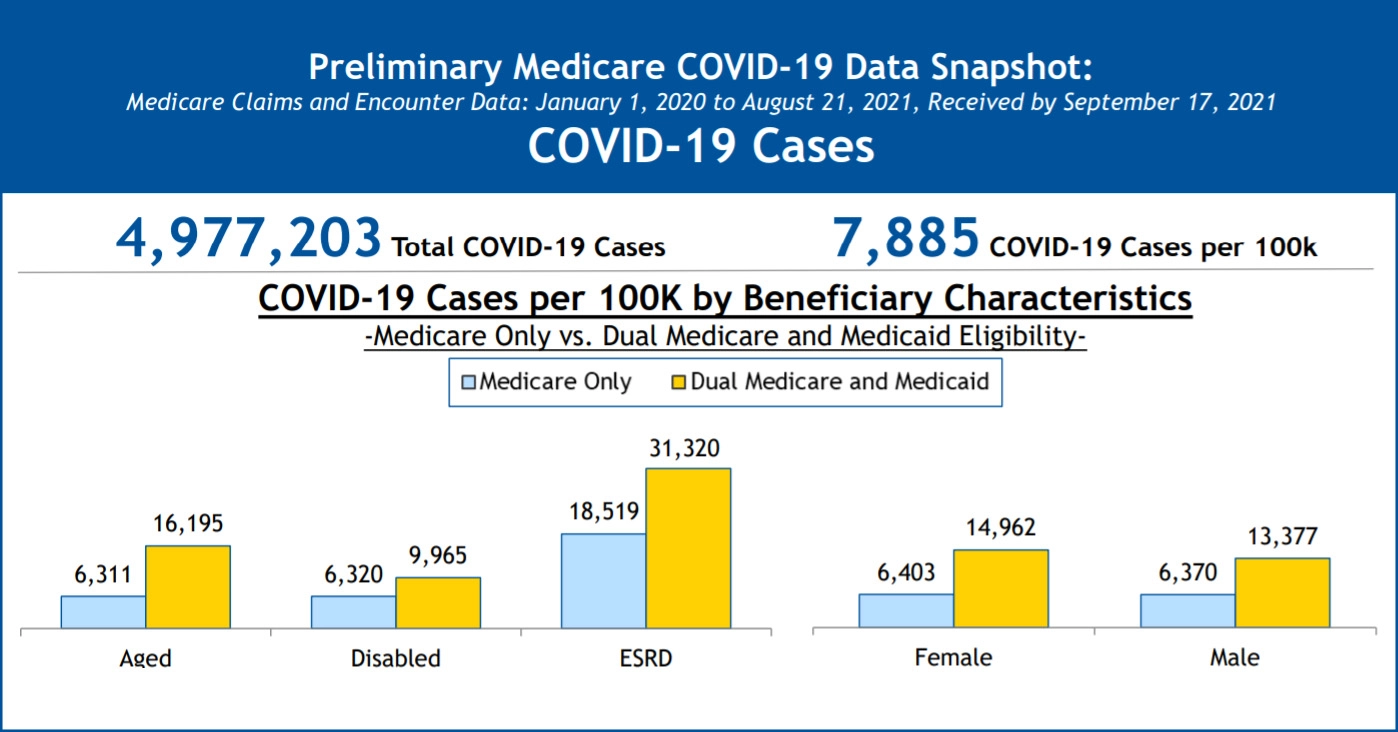
The challenges of health disparities for dual eligible members have only grown worse through the ongoing COVID-19 pandemic and several variant outbreaks. In fact, compared to individuals exclusively covered by Medicare, D-SNP members have a higher probability of contracting the virus and are approximately 2.6 times more likely to be hospitalized due to COVID-19 complications.1
As dual eligible individuals often have complex care needs and chronic conditions that are susceptible to heightened risk, the dangers of erroneous hospital utilization are obvious. According to Health Management Associates, “Dually eligible individuals also make up the majority of long-term stay nursing facility residents, which surpassed 123,000 COVID-19 deaths as of May 2021.”1
Recent CMS (Centers for Medicare and Medicaid) data further confirms that COVID-19 related hospitalization trends for dual members have notably exceeded those of individuals covered solely under Medicare (see image below).
Using technology to engage D-SNP members
Technology intervention tools are improving coordination, churn, and engagement – supporting both dual eligible members and the plan.
Scalable technology to strengthen models of care
Of course, the success of every member’s health trajectory is of top importance to the plan. So how can payers support the entirety of their D-SNP populations, including members who are ineligible for care management, when adding staff and compromising the budget is out of the question? When we scale out to see the bigger picture, the true poison to member engagement becomes clear: members are eminently and pervasively lonely.
Technology on its own is by no means the solution to loneliness for underserved populations. It is, however, the means by which humans are better able to reach and support lonely members.
The Pyx Health program takes continuity of care a step further by
blending app technology with consistent human companionship to keep members engaged while alleviating additional burden on the health plan staff. A recent Pyx Health study revealed that among a control group of D-SNP members utilizing the program, 82% scored a 4 or 5 (5 being the highest) on how connected Pyx Health made them feel to their health care team.
Technology solutions for disabled and homebound members
Many dual-eligible individuals with disabilities are less mobile and have greater challenges leaving the house to access necessary benefits and medical assistance, often unaware of the resources available to them. Technology interventions make it easier for the member to alert the plan of their needs. Using low data technology 24/7 at the touch of a finger, Pyx Health is executing timely referrals from the members to their plan by coordinating resources to durable medical equipment and in-home care services.
Health plans are also waking up to the necessity of ensuring that member based tech is designed to specifically accommodate physical and intellectual disability needs. If the member is unable to read or operate technology in the way it is intended, it is yet another wasteful venture. Pyx Health technology is both readability and accessibility-friendly to comply with usability for members with various special needs. Members who are unable to manage technology altogether still reap the benefits of human companionship and connection to plan resources by building trusted relationships with the Pyx Health Compassionate Support Center over the phone.
Avoid unnecessary inpatient and ED utilization with SDOH interventions
While health risk assessments capture an initial snapshot of a member’s condition, their future state is indisputably uncertain. Properly supporting members means monitoring needs with a whole-person care approach to get ahead of worsening chronic conditions with the potential for crisis escalation.
Predictive member-based technology software, including Pyx Health empathetic technology, is being used to flag potential high-risk individuals, alerting the plan, and connecting the member to accurate resources in precise moments of need. Pyx Health data found that within the control group of D-SNP member users, those who indicated an SDOH need were much more likely to also report loneliness on the UCLA-3 screening. The correlation between loneliness and insufficient resources is no coincidence, further driving home the importance of companionship and active connection to the plan.
Self-reported in-app evidence-based screenings paired with ongoing human support enhances the care management process by connecting members back to appropriate health plan services — improving quality of life both inside and outside of the traditional setting. Of Pyx Health D-SNP members who spoke to the Compassionate Support Center staff (an “ANDY”), 75% reported that the calls helped them avoid a higher level of service such as a visit to an ED, calling 911, or a crisis line. As a result, plans are improving CAHPS and STAR ratings by increasing engagement and quality of care for their members.