For decades, health care leaders have worked tirelessly to improve and evolve patient care – experimenting with solutions to adequately engage and account for the diverse needs of underserved populations. Now, after facing health equity roadblocks impacting outcomes and contributing to approximately $93 billion in excess medical costs3, payors are coming home to a truth that has been a fundamental component in solving some of their biggest problems – hidden in plain sight yet present all along.

It is one that shows no bias for age, race, ethnicity, gender, or socioeconomic status. No matter what you look like, identify as, or where you come from, there is one element within us all that drives everything we are, and therefore the repercussions in its absence: connection. Our internal interconnected systems of mental, physical, and behavioral health are directly reflected in our need to engage and connect in all aspects of our lives.
The health care industry is striving to emerge beyond what it has been in the past. It is becoming more than going to a clinic for a routine appointment and getting a written prescription – it requires seeing the whole person. From this vantage point, the obstacles and disparities that specific populations face in comparison to others become obvious. Plans are recognizing the debilitating feelings of loneliness and isolation that accompany their members’ inequities and the consequences for all.
Advancing health equity: Health disparities strategy
Whether it be genetics, income, race, ethnicity, geographic location, or physical limitations – innumerable factors inform health outcomes. Calculating key drivers of disparities for each member and implementing a health equity strategy takes a comprehensive approach because, naturally, humans are complex beings. Technology and human companionship can serve as the guiding light in whole-person care models – reminding members that they are not alone in the struggles they face.
Loneliness is vastly present among vulnerable populations experiencing health inequity – often intensifying barriers to sufficiently engaging individuals in their own health care. Volumes of research have exposed the lethal nature of loneliness and social isolation on health outcomes – inspiring the formation of new models to address disparity-related social health risk. Plans are now taking action to integrate loneliness solutions into their health disparities strategies as data continues to confirm the impact it has on member success outcomes.
Social determinants of health and health disparities
Screening for social determinants of health (SDOH) provides deep insight into an individual’s quality of life. Thus, when a member faces a disparity, a social or economic-related need is indicated and often impacts health outcomes. Higher social determinants of health needs are correlated with high levels of loneliness. According to Pyx Health data, members who are lonely are reporting challenges with food, housing, and income, at 2 to 5 times higher rates than those who reported having supportive social networks. For instance, if a member does not have the ability to purchase a shower chair due to income limitations, they are more prone to neglect their hygiene and experience a health decline on multiple levels.
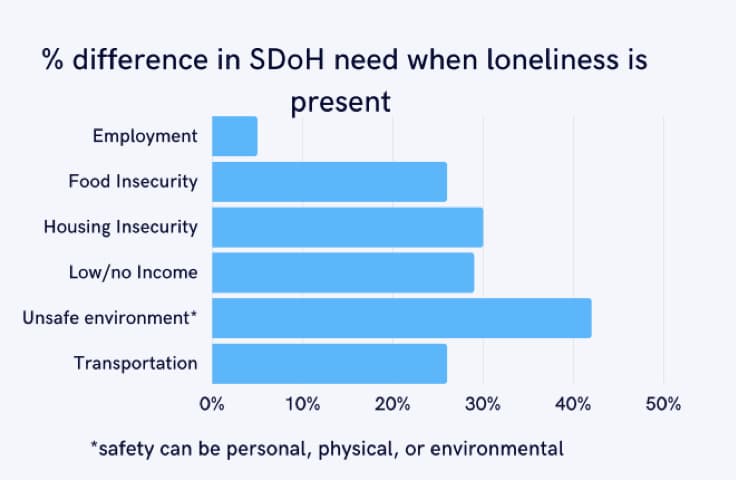
Additionally, safety concerns for lonely members are at the highest of all populations that Pyx Health serves. Pyx Health found a health plan client’s members were 110 percent more likely to identify a “safety” SDOH need when they are lonely. Pyx Health and their health plan partners are examining the types of safety issues members have such as domestic violence or risk of falling. Utilizing predictive engagement tools can support plans in tailoring the care approach to the member and their specific needs.
To alleviate the burden on the member and their health care team, Pyx Health’s Compassionate Support Center staff provides companionship to the member in moments of need. By pairing technology and human connection, Pyx Health regularly screens for SDOH needs and loneliness – making referrals back to the health plan and relevant resources to ensure members are adequately served.

Health equity, data collection, and whole person care
Evaluating risk profiles and understanding root causes of disparities for each individual member can seem like an insurmountable task. Health care technology and data collection are vital pieces in monitoring needs as well as providing calculated foresight into population trends. Data that provides a holistic scope of the member and derives a projected future outcome is essential in getting ahead of crises moments.
Pyx Health collects a compilation of data insights from member files supplied by the health plan as well as self-reported screenings, verbal interactions, and in-app activity from the member. Some examples of data we utilize are race, ethnicity, language, gender, housing needs, unsafe environments, income gaps, and food insecurity.
As the Pyx Health team monitors indicators of users with a higher propensity of loneliness, key learnings provide the health plan executives greater awareness into their members – so both sides feel more connected. If we can identify people and support who are lonely, we can also help them solve their SDOH needs to close gaps driven by disparities.
Health disparities: Diversity and inclusion
Better serving vulnerable populations through the hardships of inequity takes actively working to understand cultural and socioeconomic biases. Excluded and marginalized groups face discrimination, segregation, and other prejudices that greatly contribute to feelings of disconnection. Efforts to include diversity and inclusion practices into health care can deepen the members’ feelings of connection to their plan.
Pyx Health intentionally hires diverse ethnic, race, gender orientation, age and education levels. The staff also trains in diversity and inclusion practices on an ongoing basis. Members find that their Pyx Health Compassionate Support Center companions can often relate to adversity they have experienced, building trust and member satisfaction. Data shows that 83 percent of Medicaid members who use Pyx Health technology and services report feeling more connected to their health plan.
Rather than retrofitting the product to fit the needs of Medicare and Medicaid beneficiaries, Pyx Health technology was built with the end user in mind. Content and resources are specifically designed with cultural sensitivity to support populations such as LGBTQ+, foster care, care givers, low income, uniquely abled, and more.
Equity of access to health care services
From the member’s perspective, disparities that cause difficulties accessing health care services are often met with frustration, shame, and a feeling that they are alone in getting necessary care. Understanding common barriers influenced by social, environmental, and economic factors can inform the tactical approaches to the plan’s health disparities solutions.
Ethnic and racial disparities in health care
As a byproduct of historical racism and discrimination, marginalized groups have felt the impact of loneliness. Inequitable health complexities are largely associated with race and ethnicity. A recent study indicated that the average lifespan of African Americans is 3.5 years shorter than White Americans as a result of socioeconomic and health disparities.1 As research continues to prove higher mortality, morbidity, and social disadvantages, the truth between the lines is that they are also losing family, friends, and social connections at a higher rate than others.
These grievances and stressors on social health are also influencing the ability to properly engage in care. In fact, in comparison to white older adults, racial and ethnic minority older adults tend to have less equitable access to health and social service resources.1 Raising awareness in public and private sectors is necessary to confront racial inequities.
Technology and health disparities
A common misconception is that low income members do not use technology due to low income and socioeconomic factors. The reality is that 86 percent of adult Medicaid beneficiaries own smartphones and 69 percent own tablets at nearly the same rates as the general adult US population (approximately 86 percent and 72 percent).2 As government issued devices are often supplied to Medicaid and Medicare beneficiaries, it is not getting access to the technology itself that is the common barrier. The inequities are often due to impairments, limitations, and other external factors that create an inability for members to utilize features within the technology.
In order to mitigate technology and broadband barriers, Pyx Health technology, including our app features, are specifically designed for low data usage. The application itself is both readability and usability friendly to accommodate physical, cognitive, and intellectual disabilities that create technology disparities. Additionally, it is offered on both app stores and as well as a Progressive Web App (common URL) to be accessible on all device types and operating systems. The Pyx Health features and tools are tested on government issued devices and low bandwidth environments to verify quality of experience.
Poor health literacy as a barrier to patient care
Educational inequities and language barriers are highly prevalent among vulnerable populations – creating obstacles for the member to understand care compliance and after-care procedures.
Offering comprehensive tools to address health literacy is an effective way to reduce uncertainty and support the member’s participation in their care. Content within the Pyx Health application abides by the CMS 6th grade reading level requirement. The app also provides language options for both English and Spanish speaking users.
For members who prefer receiving support over the phone, Pyx Health offers companionship from bilingual speakers (Spanish and English) of the Support Center staff. The team also supports the relationship between the member and their health care team by making referrals to necessary translation services.
Bridging access to care 24/7
 Members who experience health disparities often face limitations to engaging with their plan benefits in moments outside of the traditional care setting. Pyx Health data shows that members who report as lonely also engage with the application in the middle of the night.
Members who experience health disparities often face limitations to engaging with their plan benefits in moments outside of the traditional care setting. Pyx Health data shows that members who report as lonely also engage with the application in the middle of the night.
The Pyx Health call center has extended support center hours so that personnel are available evenings and weekends. Members also always have access to hotlines, screenings, and scheduling options 24/7 through the Pyx Health app.
To learn more about how the Pyx Health solution is engaging vulnerable members of various populations and saving plans an average of $5,083 per member over 6 months, download the white paper below!
References
- Examining Rural and Racial Disparities in the Relationship Between Loneliness and Social Technology Use Among Older Adults https://pubmed.ncbi.nlm.nih.gov/34532308/#:~:text=The%20primary%20study%20results%20demonstrated,loneliness%20than%20urban%20older%20adults
- Deloitte Insights – Medicaid and digital health https://cookcountyhealth.org/
- Kaiser Family Foundation – Disparities in Health and Health Care: 5 Key Questions and Answers https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question-and-answers/



